Biotherapy International
The Center for Innovative Cancer Immunotherapy & Cellular Therapy
“Biotherapy International applies the latest fundamental scientific advances at the patient’s bedside to save lives and improve the quality of life of every patient.”
The Smart Immunotherapy for Cancer Patients
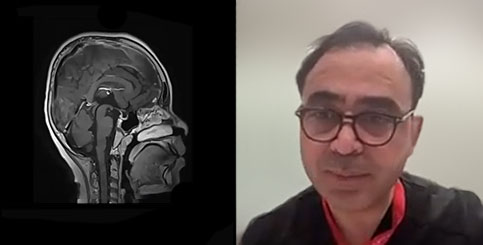
At Biotherapy International, patients receive personalized cancer treatments based on innovative immunotherapy techniques. We cannot guarantee the success of every cancer patient. However, by offering “smart” rather than aggressive cancer treatments, we promise to do our best to help the patient recover and maintain their quality of life.
Mesenchymal Stem Cells (MSC) in the Regenerative Medicine
The methods of regenerative medicine used at the Biotherapy
International clinic can achieve significant results in the treatment
of diseases of the immune system, neurodegenerative diseases, trauma and many other diseases, when the possibilities of conventional medicine have been exhausted.

Our Team
The multidisciplinary team at Biotherapy International is an integrated group of caring professionals who have dedicated their lives to treating patients with cancer and other serious conditions. Biotherapy International physicians and researchers are internationally renowned for their groundbreaking innovations and treatment methods.