Natural Killer Cells: A New Anti-Cancer Tool
For the first time in several decades, immunotherapy has opened the gates for an entirely new family of anti-cancer treatments. Radically different from traditional chemotherapy or radiotherapy, anti-cancer immunotherapy encompasses different types of precision medicine and puts the patient’s immune system at work directly against cancer.
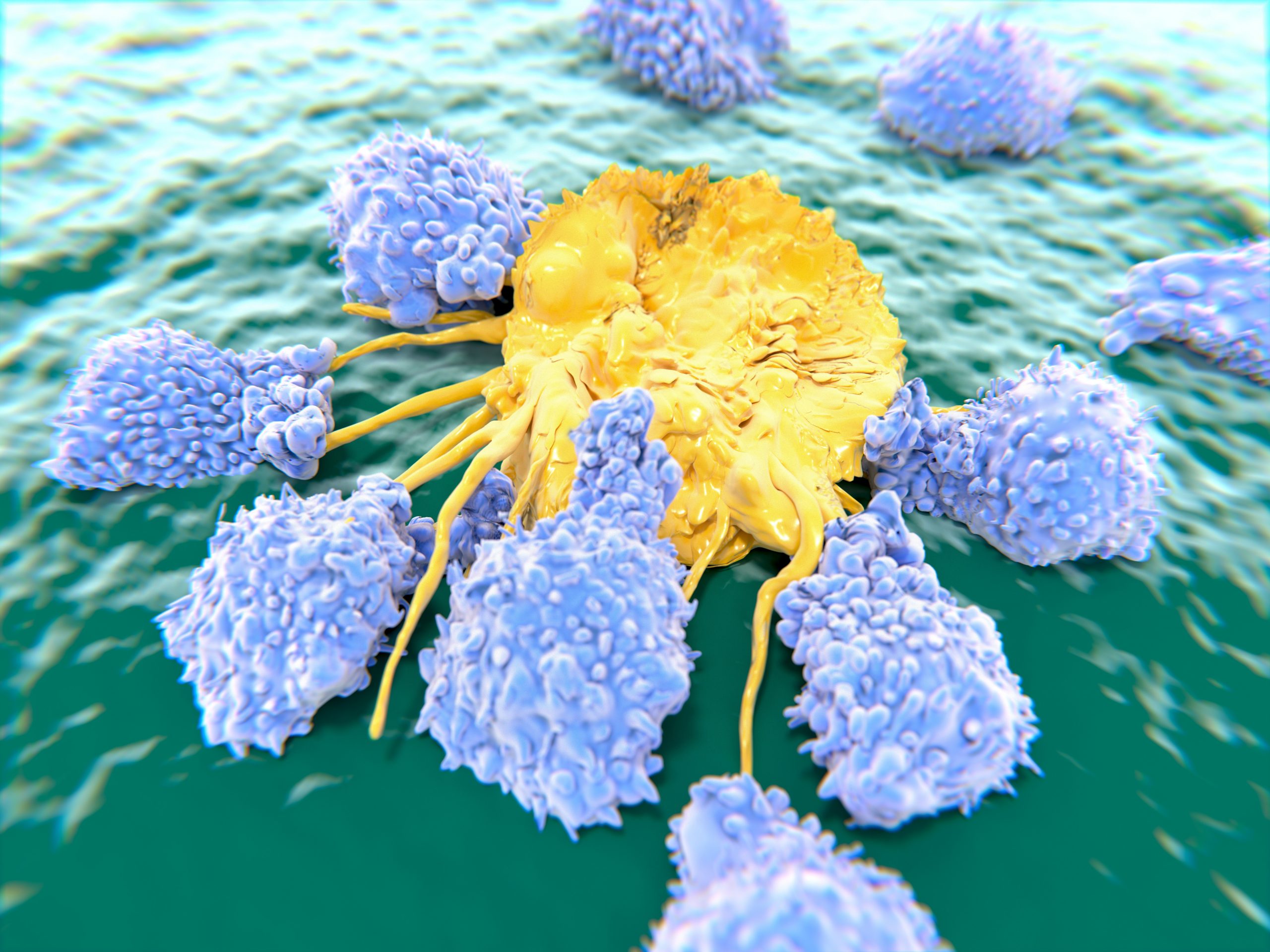
These treatments can be designed through a handful of different methods. Out of them, the use of Natural Killer (NK) cells is proving to be an aggressive form to “chase” tumor tissue that has developed resistance, even if it has spread to different parts of the body.
NK cells are a new method for immunotherapy.
What are Natural Killer Cells?
Also known as NK cells, Natural Killer cells are a specific type of granular lymphocyte – one of the cells in charge of preserving innate immunity. They are closely related to T and B cells but can trigger a faster response after identifying an “invading” agent. They comprise up to 15% of all the body’s immune cells
NK cells are granular. That is, they have small rough particles on their surface, which allow them to enter and attack tumor cells. At the same time, NK cells also accomplish other tasks within the immune system:
- They patrol the body through the bloodstream, detecting the makeup of any cells they come into contact with.
- Act as a “memory storage” where the body can preserve information on past immune reactions.
- They secrete cytokines, stimulating other immune cells, such as dendritic cells or macrophages.
How can Natural Killer Cells Attack Cancer Cells
Natural Killer cells have the innate ability to attack mutated cells spontaneously without the need to be “activated.” However, in many people, this ability is turned off by the presence of inhibitory receptors, which normally prevent NK cells from indiscriminately attacking healthy cells.
However, many types of tumor cells do not have this inhibitory effect. When this happens, NK cells will begin excreting cytokines such as interleukin or interferon. Both cytokines can attach themselves to specific receptors within cancer cells. Once they enter, they trigger a process known as cell apoptosis –programmed cell death that begins from within the cell.
In some cases, mutated cancer cells will nonetheless manage to inhibit the activity of NK cells. In others, the cells themselves will fail to recognize some types of mutations, allowing cancer to grow, or the tumor will be too large for the available amount of NK cells in a patient’s body.
When this happens, we can still activate NK cells externally, “retraining” them to ensure they accomplish their task. In addition, we can supplement the amount of circulating NK cells using donor tissue.
How does Natural Killer Cell Treatment Work
Natural Killer Cell therapy may encompass three different stages, depending on the patient’s clinical condition and the specific characteristics of the tumor.
The first stage involves acquiring enough NK cells to infuse the patient. These cells are often harvested and isolated from umbilical cord blood. After isolation, the highest-quality ones will be selected for further cultivation.
The “premium” cells will be expanded and activated during the next stage in the lab. Ideally, treatment will require using approximately 3 to 10 million cells per kilo of the patient’s body weight. At this stage, their effectiveness for a specific cancer type can also be tested, assuming fresh or cryogenically-frozen tumor tissue is available.
Finally, the end NK cell product will undergo another round of quality testing. Then, it will be administered to the patient via intravenous (IV) injection.
The Full Extent of the Promise lies Ahead
Natural Killer Cell’s ability to trigger “cell suicide” on specific mutations while leaving surrounding tissue untouched is one of the most promising niches in anti-cancer therapy. Although NK cell treatment is still not widely available as part of the “standard of care,” it has shown to be a flexible method that can be combined with both traditional therapies and other experimental immunotherapy.
