Anti-cancer immunotherapy is a type of treatment that stimulates the body’s immune system to fight malignant tumor cells.
With traditional cancer treatments, patients are often able to achieve a state of minimal residual disease, where only a small number of cancer cells remain in the body. However, some types of cancer are resistant to standard treatments. Additionally, cancer cells can spontaneously mutate, especially after prolonged exposure to chemotherapy, leading to the development of progressive multi-drug resistance.
Every malignant cell originates from so-called “cancer stem cells” found within a tumor. The cancer stem cells’ resistance to chemotherapy and radiotherapy can explain why numerous applications of these treatments can be unsuccessful in preventing disease progression and recurrence.
The Role of Immunotherapy in Cancer Treatment
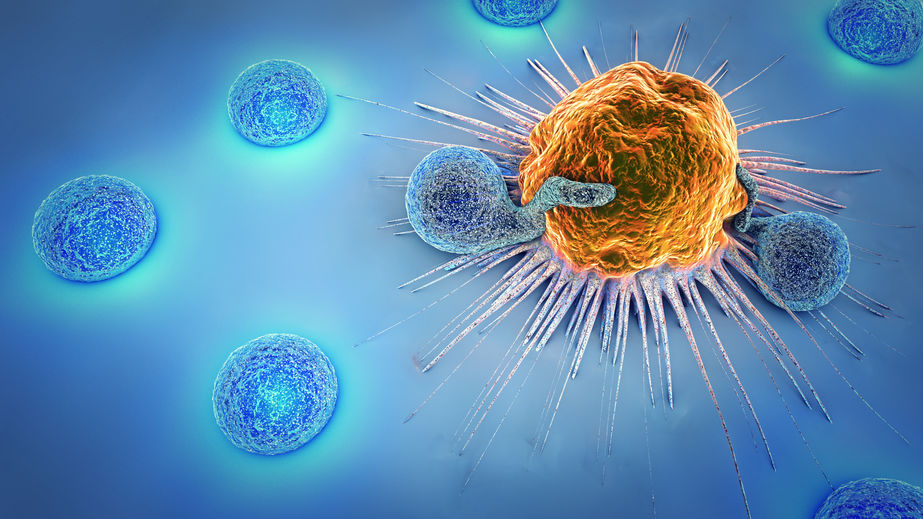
The immune system’s primary function is to recognize and destroy all foreign agents, including cancer cells. Since malignant tumors develop from the mutation of a single cell, complete cancer eradication requires the destruction of every single malignant cell. Unfortunately, conventional methods often fail to accomplish this. When conventional treatment options are exhausted, negative outcomes become inevitable.
Cancer immunotherapy, by enhancing the immune system’s ability to recognize and destroy malignant cells, is one of the most promising treatment for cancer.
Several mechanisms actively suppress the response of the immune system to cancer, and so immunotherapy takes a multi-pronged approach to address this.
Cancer immunotherapy focuses on three main objectives:
- Elimination of all factors that suppress the activity of the immune system.
- Activation of the body’s natural anti-tumor mechanisms.
- Enhance the action of immunotherapy with the use of drugs with scientifically proven anti-cancer efficacy.
Using immunotherapy to combat cancer can be likened to a real-life battle. If the number of “fighters” (immune cells) exceeds the number of “enemies” (cancer cells), or if your “fighters” are better trained and better armed, the likelihood of winning the battle increases. On the other hand, if cancer cells multiply faster than immune cells and their ability to “kill”, there is a chance that the fight against cancer will be lost.
Treating cancer with immunotherapy enables the immune system to identify and destroy cancer cells. For example, activated donor killer cells administered to the patient can destroy cancer cells with multi-drug resistance, even in cases of malignant neoplasms considered incurable.
Therefore, immunotherapy plays a crucial role in cancer treatment, especially when applied after traditional treatment methods at the minimal residual disease (MRD) stage, where a small number of cancer cells remain in the body.
Cancer Treatment with Immunotherapy: Hope for a Cure
Reduced activity of a patient’s lymphocytes contributes to cancer therapy failure, and can be caused by a combination of three factors:
- Antigens of cancer cells, which differentiate them from healthy cells, have low immunogenicity, meaning they elicit a weak immune response.
- Cancer leads to an increase in cells that inhibit the anti-tumor activity of the immune system.
- Development of resistance or tolerance to malignant cells, which mimic “healthy” cells, leading the immune system to no longer recognize them as foreign.
For successful cancer treatment using immunotherapy, a comprehensive approach is needed to address all these factors.
Firstly, enhancing the ability of cancer cells to trigger an immune response can be achieved by using interferons. Interferons are proteins made in the body that increase the production of cellular antigens (foreign agents recognized by the immune system). Antigens that attach to cancer cells can be used to make them more recognizable to the immune system. “Tagging” with new antigens can transform them into cancer vaccines, as we will explain in detail later.
Secondly, the success of immunotherapy depends on eliminating mechanisms that suppress the immune system’s function. Low doses of cyclophosphamide and checkpoint inhibitors (e.g. ipilimumab, nivolumab, or pembrolizumab) are prescribed for this purpose.
Thirdly, it is necessary to overcome the immune system’s resistance to cancer cells by using cancer vaccines or by introducing deliberately mismatched donor lymphocytes that transform into active killer cells. Such mismatched donor lymphocytes, including T cells and natural killer (NK) cells, target cancer cells specifically by using monoclonal antibodies. Activated mismatched donor lymphocytes are the most effective method of destroying resistant cancer cells through a mechanism resembling organ rejection.
Innovative Types of Anti-cancer Immunotherapy
One of our most promising treatments for cancer patients involves the use of oncolytic viruses. An oncolytic virus is harmless to healthy, normal cells. It can kill cancer cells directly or activate the patient’s immune system to attack cancer cells.
Another potentially effective treatment is Coley’s Toxins. It is a mixture of bacterial toxins created over 120 years ago by Dr. William Coley. Coley’s Toxins activates systemic immune reactions, leading to the regression of malignant tumors. The toxin can be administered directly into the tumor site or used in creating cancer vaccines.
Cancer vaccines are another scientifically proven method of cancer immunotherapy. Each vaccine is individually tailored based on the patient’s tumor cells. Tumor samples obtained during surgery and cryopreserved in the Tumor Bank are used to develop the vaccines. By using Coley’s Toxins or oncolytic viruses, cancer cells that were previously unable to activate the patient’s immune system can be made more “recognizable.” After treatment with Coley’s Toxins or oncolytic viruses, cancer cells begin to actively produce foreign substances — antigens — that distinguish cancer cells from similar normal cells.
Another therapy method is Allogeneic Targeted Activated Cancer Killer Cells (ATACK). A combination of deliberately mismatched killer cells (T cells, NK cells, and NKT cells) helps destroy the tumor through a mechanism resembling rejection. Monoclonal antibodies against antigens produced on the surface of these cancer cells are used for preferred targeting of specific cancer cells.
Personalized Protocols for Anti-cancer Immunotherapy
At Biotherapy International, we not only believe that cancer can be treated but also that it can be cured, provided that the principles of optimal treatment are fully adhered to. In cases where complete cure is not possible due to late diagnosis, we prescribe non-aggressive treatment methods to slow disease progression and maintain the patient’s quality of life.
Biotherapy International treatment protocols are based on fundamental scientific concepts and the findings of preclinical and clinical studies, including non-standard procedures not yet included in official recommendations.