The first successful cure of a patient with a fulminant relapse following myeloablative stem cell transplantation using donor lymphocyte infusion
Allogeneic stem cell transplantation is considered the most effective treatment of otherwise resistant blood cancer. Patients with recurrent disease following successful myeloablative allogeneic stem cell transplantation were nearly always considered incurable. A simple cell-mediated treatment of relapse following allogeneic stem cell transplantation developed by Prof. Slavin changed the dogma and confirmed that many patients relapsing following successful allogeneic stem cells transplantation may be cured by a simple procedure called donor lymphocyte infusion (DLI).
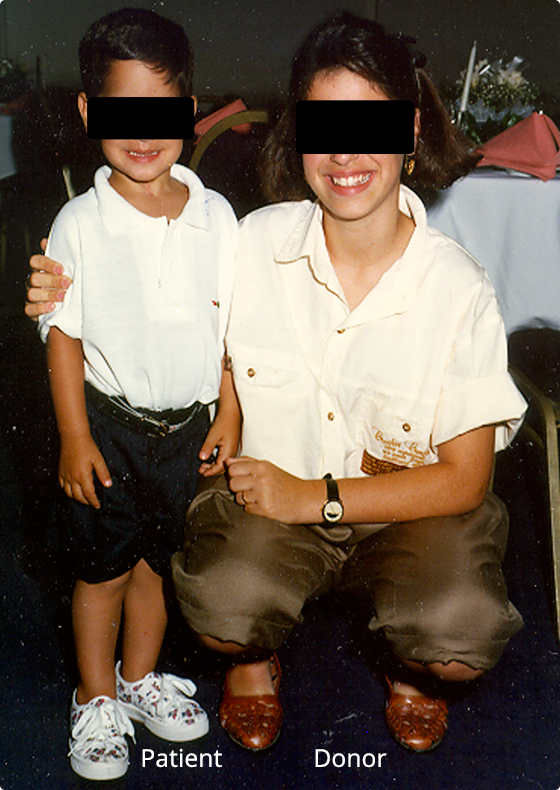
On the left, we show the first patient successfully treated and cured following failure of a very aggressive myeloablative combination of chemotherapy and total body radiation. His donor is on the right.
The story began when the mother of this patient, who was 30-months-old at that time, approached Prof. Slavin in 1986 to treat her son. He had been deemed incurable at another major medical center in Israel. He had been diagnosed with poor risk pre-B ALL, had relapsed on therapy twice, then presented with a fully-resistant 3rd relapse with no hope to respond to any known treatment.
Although it was clear his aggressive leukemia could not be controlled even through a conventional myeloablative transplant procedure, the mother asked and insisted to provide the last hope by using allogeneic stem cell transplantation. Considering the need to eradicate fully resistant leukemia with wall-to-wall infiltration of leukemic blasts in the blood and in the bone marrow, the protocol chosen by Slavin consisted of the most aggressive conditioning ever offered to any patient, consisting of 4 times the lethal dose of whole-body radiation delivered from a high dose-rate linear accelerator, in addition to 3 different chemotherapy combinations prior to rescue with his sister’s bone marrow cells.
Luckily, the patient survived the transplant procedure and was fully reconstituted with his sister’s cells. Leukemia cells were no longer visible, and it seemed for a while that the leukemia was completely eradicated. Unfortunately, a few weeks later, the patient was brought to the emergency room gasping for breath due to an obstructive mass in the upper airway tract, with visible lesions on his forehead like a unicorn and 3 additional extra-medullary lesions with blood and bone marrow massive infiltration with leukemic blasts.
An emergency tracheotomy was done. At that stage, it was clear that there was no chance for any additional effective treatment, so the mother preferred to take the patient home for as long as he would last. Three days later, based on experiments done by Slavin in an animal model of lymphocytic leukemia, he called the mother and suggested a simple experimental treatment as a last resort, suggesting that due to engraftment of donor stem cells, the rejection of alloreactive donor lymphocytes could be prevented and result in the induction of graft-versus-leukemia (GVL) effects.
Accordingly, an infusion of 20ml of freshly obtained blood from his sister was injected intravenously and the patient was sent home. A week later, after confirming he was still alive, the procedure of 20ml fresh blood infusion was repeated a second time. Later on, new injections were performed of 20ml of fresh blood each every week or two, for a total of 6 times.
Although such patients are never expected to respond to any available treatment, the patient responded dramatically, with gradual disappearance of all visible tumor masses including the lesion that obstructed his airway in the trachea. In parallel, all leukemia blasts disappeared and all patient’s leukemic blasts were replaced with normal donor’s (female) cells.
To date, 34 years later, this patient is alive, well and has never required any additional medical treatment since then. This is the first patient ever successfully treated and cured despite 100% resistant disease following the failure of maximally-tolerated myeloablative conditioning and allogeneic stem cell transplantation. The procedure used for treatment since then is known as donor lymphocyte infusion (DLI).
DLI was confirmed effective in eradicating malignant cells that are fully resistant to lethal doses of chemo-radiotherapy following allogeneic stem cell transplantation. This happened at many transplant centres worldwide. DLI is also considered for prophylactic treatment against relapse in patients with high-risk disease. Furthermore, the anti-cancer effects of alloreactive donor lymphocytes, DLI, could be further amplified by activation of donor lymphocytes with interleukin 2 (IL-2).
The patient’s successful cure, and that of those who followed, provided a clear indication that smart immunotherapy could be much more effective than any available anti-cancer treatment. Accordingly, the use of activated donor lymphocytes resulted in development of new therapeutic strategies for treatment of cancer focusing on smarter cellular therapy rather than relying exclusively on more aggressive and consequently more hazardous non-specific chemo-radiotherapy.

